Estimated reading time: 6 minutes
Whether your practice books 20-minute, 30-minute, or 90-minute appointments, there are common challenges and hurdles that come with booking, managing, and coordinating time between your business, its providers, and each and every one of your patients. No matter how you look at it, taking on the challenge of improving the patient scheduling process is daunting.
We’ve written before about the many drawbacks and pitfalls that come with scheduling. No-shows, late arrivals, mix-ups, and overbooking are just a few of the most prominent issues.
The room for error is also enormous.
Most importantly, each of these small mistakes can have major consequences for your business and your patients.
No one-size-fits-all scheduling process will remove all the stress and uncertainty of running a practice. Instead, you can re-engineer how you manage appointments to create a streamlined, reliable, and predictable system that works for everyone.
Deconstructing the scheduling process
Of the four stages in problem-solving, generally, the most difficult is the first step: identifying the problem you are trying to solve.
In the case of the patient-scheduling process, this is best accomplished by first deconstructing the entire patient experience.
Identifying the outcomes you want to achieve (e.g., shorter patient wait times) is simple enough. But to identify the problems you need to solve first, you’ll have to begin by deconstructing and analyzing how your patients interact with your practice.
Using design thinking and lean strategies, you should first map out each step in the patient process, from initial contact to post-appointment follow-up appointments.
This is critical in developing a streamlined approach to improve patient scheduling.
Having a grasp of the entire experience will allow you to identify the bottlenecks in your current system. You can then optimize the experience to provide a better patient experience, improve efficiency, and reduce complexity for your practice.
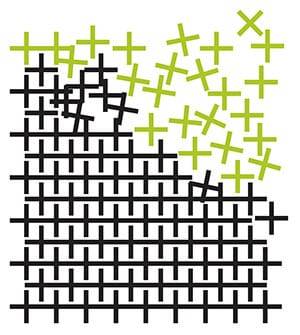
Check out this idea in action in the Journal for Healthcare Quality’s article on using the lean methodology to improve patient scheduling (Figure 3).
While this process can seem complex and daunting, the reality is that it’s rather straightforward.
There are many devices, systems, and processes you can use. But it essentially comes down to four basic steps:
- Identify key patient needs and goals.
- Walk through several patient interactions, noting each step of the process.
- Create a diagram showing each of the touchpoints and describing their nature.
- Critically analyze each touchpoint to identify problems, bottlenecks, and opportunities for improvement.
Using this approach, you can consider the big-picture view of the patient’s journey and zoom in on each interaction to understand its role in the larger experience.
Schedule optimization
For most practices, different types of appointments require different amounts of time and attention.
Unfortunately, many practices also miss the opportunity to strategically prioritize and organize these different appointment types. This leads to challenges and inconsistencies, with complex appointments being scheduled for inopportune time slots or without proper consideration for the time needed in that particular case.
It’s important for your practice to establish clear guidelines regarding when and how to schedule certain types of appointments, accurately assess a particular case, and identify its type and scope.
This process goes hand in hand with the in-office and over-the-phone triage that is likely handled by front-of-the-house staff.
The most common approach for improving this process and optimizing appointment schedules is developing an in-house chart to evaluate specific cases. The chart can be used to score cases according to relative urgency and estimated appointment length.
Staff who are responsible for setting and managing appointments can refer to these charts to assess a client’s needs and take the appropriate course of action.
Lastly, it may make sense to implement a strategy in which your practice will prioritize more complex or lengthier visits while referring out other types of appointments.
From a business standpoint, this may allow you to schedule fewer appointments while maintaining a predictable flow of patients and revenue.
Measuring success
The next phase of building a streamlined patient scheduling process is to have a feedback mechanism for the entire system.
While all this pre-planning and design can help give shape and structure to the best practices, you need real-world data to continue improving over time.
Did appointment type A actually take 30 minutes as planned? Or did it take 45?
Your practice needs to have a process to review and analyze past appointments based on the previously defined metrics. Then, you need a mechanism to circle back and make adjustments to the system as necessary. For example, you may update the assessment chart to require longer or shorter appointment times for specific cases.
At the core of building a more efficient appointment system and reducing the complexity of your appointment process, this step is likely the most important.
It’s easy enough to devise a possible solution and create new internal policies. But even the best estimates are still just that — estimates — unless they are backed up and continuously improved with real-world data.
As tempting as it may be to make a system once and never touch it again, be sure to create a process for learning and optimization.
Implementing technology
The final piece to optimizing your appointment management process is technology.
Using the right tools can improve the patient scheduling process in three core ways:
- Simplified metrics/tracking.
- Centralized patient data.
- Patient reminders and confirmation (positive reinforcement).
Each offers some small advantage in the quest for a better and more efficient scheduling process. But taken together, they represent a massive advantage to practices that want to build a smarter, more efficient system.
Apptoto, for example, can provide a central hub for recording and tracking individual appointments and patient data. In addition, the reminder and confirmation features can help boost overall appointment performance. And, of course, Apptoto appointment reminders are HIPAA-compliant.
Ultimately, it’s important to remember that when we discuss things like appointment metrics or patient data, we’re really talking about people.
That’s one of the biggest reasons to use technology to improve your patient-scheduling process. By managing and organizing time slots less, your team can focus their energy on serving people and meeting their needs to the best of their ability.